Why This Matters
The retina is a thin, delicate layer at the back of your eye that captures light and sends signals to your brain, much like a camera sensor. If it detaches, vision becomes blurred, shadowed, or even completely lost. Retinal detachment is a medical emergency—understanding what causes it and how to protect your eyes could save your sight.
What Exactly Is Retinal Detachment?
When the retina pulls away from the layer of blood vessels that supply it with oxygen and nutrients, it can no longer function properly. Without prompt treatment, the cells begin to die, leading to permanent vision loss.
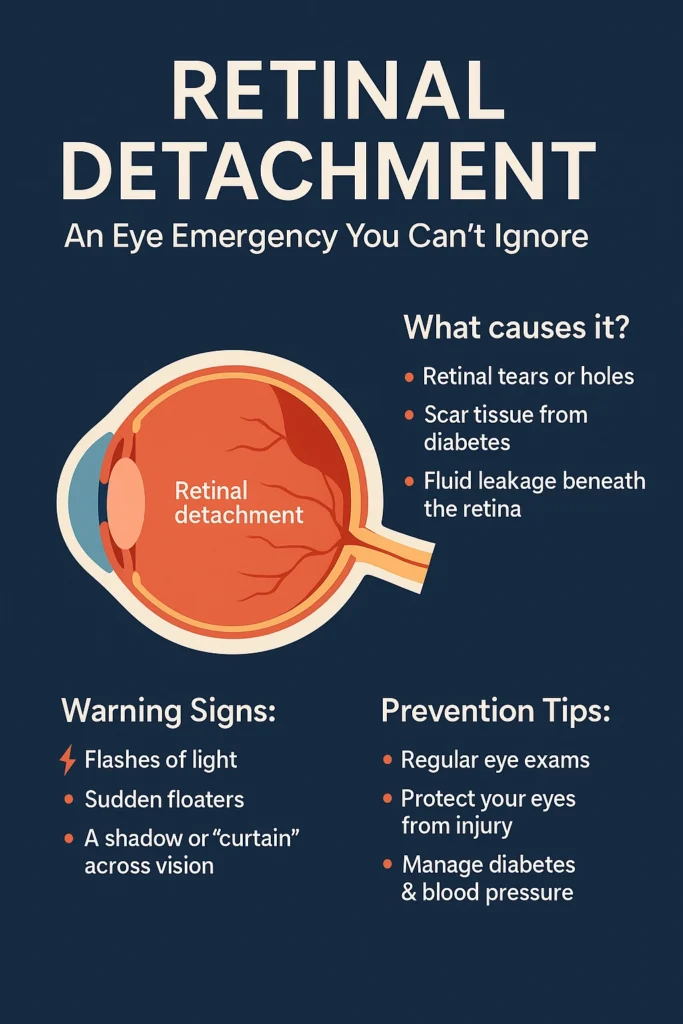
There are three main ways this happens:
- Rhegmatogenous Detachment: A tear or hole allows fluid from the vitreous gel to slip underneath, lifting the retina. Often linked to ageing changes in the vitreous, severe nearsightedness, or trauma.
- Tractional Detachment: Scar tissue inside the eye contracts and tugs the retina off its base. This is most often seen in advanced diabetic retinopathy.
- Exudative (Serous) Detachment: No tear is present. Instead, fluid leaks beneath the retina due to conditions like macular degeneration, inflammation, or tumours.
👉 For a broader overview of symptoms and treatments, see Everything You Need to Know About Retinal Detachment.
Who Is at Risk?
Anyone can develop a retinal detachment, but certain factors make it more likely:
- Age (most common between 40 and 70)
- Severe myopia (thin, stretched retina)
- Previous cataract or eye surgery
- Eye trauma or injuries
- Family history of retinal detachment
- Diabetic retinopathy and other vascular or inflammatory eye diseases
👉 If you’re living with diabetes, explore our page on Diabetic Retinopathy.
Warning Signs You Should Never Ignore
The early symptoms can be subtle, but they are your window of opportunity to act:
- Flashes of light, like streaks at the edge of vision
- A sudden shower of floaters
- Blurred or distorted vision
- A dark “curtain” or shadow creeping across your sight
If you notice any of these, contact an ophthalmologist immediately. The sooner treatment begins, the greater the chance of preserving vision.
Diagnosis: How It’s Confirmed
Your ophthalmologist may use a dilated retinal exam, advanced imaging (OCT), or ultrasound to detect tears, fluid, or scar tissue. These tests allow the doctor to pinpoint the problem and plan the right treatment.
Can You Prevent Retinal Detachment?
Not every case can be prevented, but you can reduce your risk and improve outcomes with early action:
- Have regular eye exams, especially if you’re over 40, very nearsighted, or diabetic.
- Wear protective eyewear during sports, work, or DIY activities.
- Keep diabetes and blood pressure under control.
- Respond quickly to symptoms of flashes, floaters, or shadows.
- Follow your doctor’s advice if preventive treatments like laser therapy are recommended for retinal tears.
Treatment Options
If detachment occurs, surgery is usually necessary. The right approach depends on the type and extent:
- Laser or Cryotherapy: For small tears caught early.
- Pneumatic Retinopexy: A gas bubble pushes the retina back in place, often combined with laser or cryotherapy.
- Scleral Buckle: A silicone band gently presses the eye wall inward to close breaks.
- Vitrectomy: The vitreous gel is removed and replaced with gas or silicone oil, allowing the retina to reattach.
Most patients need only one procedure, and success rates are high—about 85–95%.
Recovery and Outlook
Vision recovery depends on whether the macula (the central part of the retina) is involved:
- If treated before the macula detaches, vision outcomes are excellent.
- If the macula is already off, vision may not fully return, but surgery still prevents total blindness.
- Recovery takes time—weeks to months—and regular follow-ups are vital to monitor healing and protect the other eye.
Key Takeaways
- Retinal detachment is an eye emergency that requires urgent treatment.
- Causes include retinal tears, scar tissue, or fluid build-up.
- Risk factors range from ageing and myopia to diabetes and trauma.
- Prevention isn’t always possible, but early detection, protective habits, and regular exams greatly improve outcomes.
- With timely surgery, most patients keep useful vision.
Explore More on Our Site
✨ Your vision is irreplaceable. Don’t wait for warning signs—book a comprehensive eye exam with Dr Cronje today.

