Why Recognising Neuro-Ophthalmology Red Flags Matters
Most visual complaints you see in primary care have a straightforward cause — refractive change, dry eye, cataract.
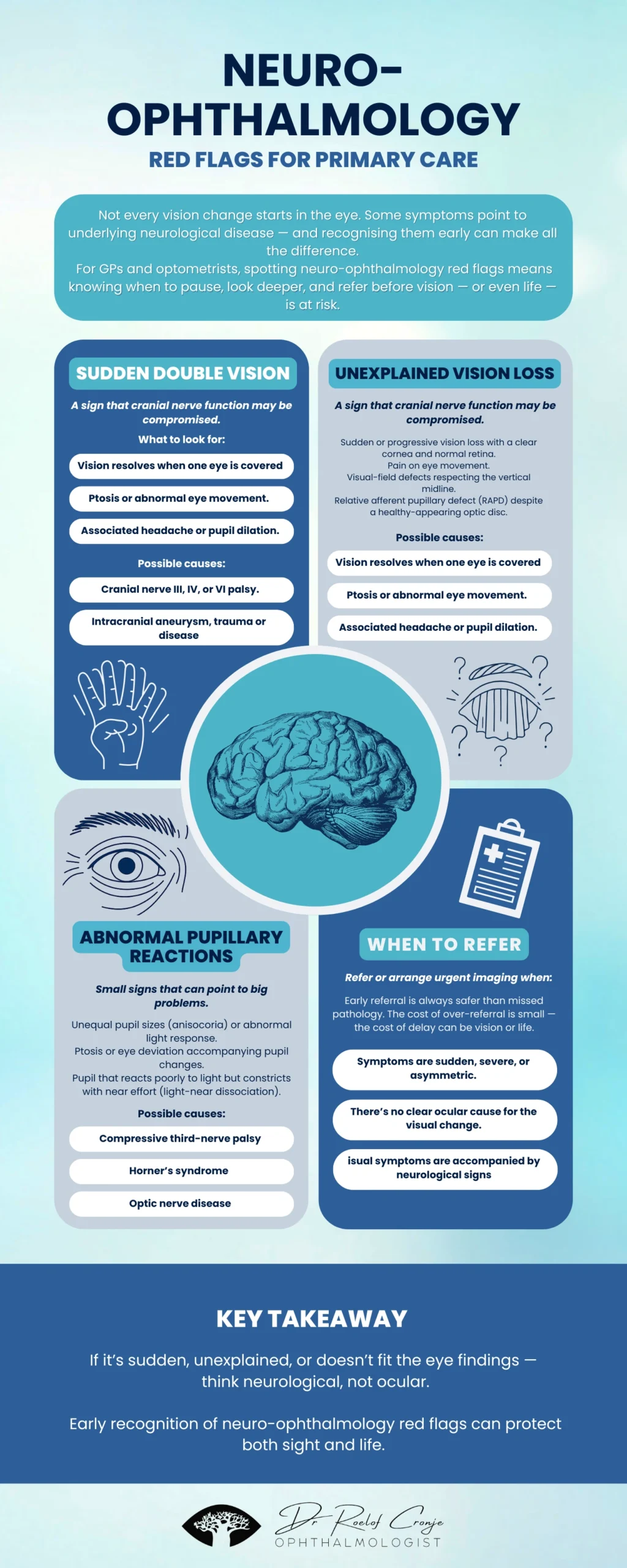
But occasionally, a vision symptom is the first sign of neurological disease. Recognising these neuro-ophthalmology red flags early can make the difference between reversible and permanent vision loss.
The challenge? These red flags are subtle, easily missed, and can precede serious underlying pathology — from demyelinating disease to aneurysm or stroke.
Recognising the difference between an ocular problem and a neurological one is key to early diagnosis, appropriate referral, and sometimes life-saving intervention.
Looking Beyond the Eye
When a patient says, “Something’s wrong with my vision,” our instinct is to reach for the slit lamp.
But if the clinical picture doesn’t fit the findings — when the symptoms are disproportionate or the eye appears normal — it’s time to think beyond the orbit.
Neuro-ophthalmology bridges this gap between neurology and eye care, and understanding its red flags helps you decide when “watch and wait” isn’t enough.
1. Sudden-Onset Double Vision: A Key Neuro-Ophthalmology Red Flag
A patient suddenly seeing two of everything is never routine.
While decompensated phoria or trauma can cause diplopia, an acute binocular onset points to possible cranial nerve III, IV, or VI palsy.
Common causes:
- Microvascular ischemia (diabetes, hypertension)
- Intracranial aneurysm or compressive lesion
- Demyelinating disease (MS)
- Brainstem infarction or trauma
What to look for:
- Diplopia disappears when one eye is covered (binocular)
- Ptosis or eye deviation present
- Headache or pupillary involvement accompanies onset
Red-flag pattern:
Painful, pupil-involving third-nerve palsy → treat as aneurysmal until proven otherwise.
👉 Refer urgently for neuro-imaging and ophthalmic evaluation.
2. Unexplained Vision Loss
When vision loss doesn’t match the ocular findings, think retrobulbar or neurological.
Possible causes:
- Optic neuritis — often demyelinating (MS spectrum)
- Ischemic optic neuropathy — vascular or giant cell arteritis related
- Compressive optic neuropathy — tumour or orbital mass
- Occipital lobe pathology — stroke, haemorrhage, trauma
Clues that it’s not ocular:
- Normal-appearing retina and clear media
- Pain on eye movement
- Visual-field defect respecting the vertical midline
- RAPD without visible disc swelling (retrobulbar neuritis)
Tip:
If the fundus looks normal but the story doesn’t fit — trust the story.
Early referral for imaging and ophthalmic review is essential.
3. Abnormal Pupillary Reactions: Subtle But Critical Neuro-Ophthalmology Red Flags
The pupils often whisper before the brain shouts.
Pupil abnormalities are subtle but powerful neuro-ophthalmology red flags.
Patterns worth noting:
- Dilated, non-reactive pupil + ptosis + eye deviation → possible compressive 3rd-nerve palsy
- RAPD (Marcus Gunn pupil) → optic nerve dysfunction
- Unequal pupils with new onset → Horner’s syndrome, Adie’s pupil, or compressive lesion
Red-flag context:
New anisocoria accompanied by headache, neck pain, or neurological deficit always warrants urgent investigation.
When to Escalate
Immediate referral or imaging is advised when:
- Symptoms are sudden, severe, or asymmetric
- There is no ocular explanation for the visual change
- Neurological signs accompany the eye findings (ptosis, weakness, speech, balance)
- There is painful ophthalmoplegia or pupil involvement
Even in uncertain cases, early referral is the safer path — the cost of over-referral is small compared to the risk of missed pathology.
Practical Approach for Primary Care
Start with three quick questions:
- Is the vision loss sudden or gradual?
- Is it monocular or binocular?
- Are there neurological symptoms?
Perform a focused neuro-ophthalmic screen:
- Visual acuity and colour vision
- Pupillary reflexes (RAPD, anisocoria)
- Ocular motility (H-test, cover test)
- Confrontation fields
Document clearly — onset, associated pain, and any systemic risk factors.
Refer early when red flags are present or results are inconclusive.
If in doubt, refer early — especially when classic neuro-ophthalmology red flags are present.
Collaborating for Patient Safety
Optometrists and GPs are often the first clinicians patients trust with visual changes.
Recognising when the story doesn’t match the findings is your cue to escalate.
Timely collaboration with an ophthalmologist ensures the right diagnosis — and sometimes, saves sight and life.
Summary Table — Neuro-Ophthalmic Red Flags
| Symptom | Possible Cause | Urgency |
|---|---|---|
| Sudden binocular diplopia with pain or ptosis | Cranial nerve palsy, aneurysm | Urgent |
| Unexplained vision loss with normal retina | Optic neuritis, ION, compression | Prompt referral |
| Abnormal pupils (new anisocoria or RAPD) | Third-nerve palsy, Horner’s, optic nerve disease | Urgent |
| Visual-field defect respecting vertical midline | Chiasmal or cortical lesion | Imaging required |
The Importance of Early Recognition
Neuro-ophthalmic symptoms can blur the line between eye and brain. For GPs and optometrists, recognising the difference is critical — because what seems like a simple vision problem can sometimes reveal a deeper neurological cause.
When you encounter sudden double vision, unexplained vision loss, or abnormal pupils, think beyond the eye and refer early. Collaboration between primary care and ophthalmology ensures the best outcomes — preserving both vision and life.
Early recognition, careful documentation, and timely escalation remain your strongest tools in protecting patients from avoidable harm.