Keratoconus is a progressive corneal condition that can quietly worsen over time. Recognising keratoconus progression red flags early allows optometrists and GPs to act before vision is permanently affected. While specialty contact lenses improve vision, they don’t stop the disease from advancing — making early referral for cross-linking or ophthalmic input crucial.
Understanding Keratoconus and Early Progression
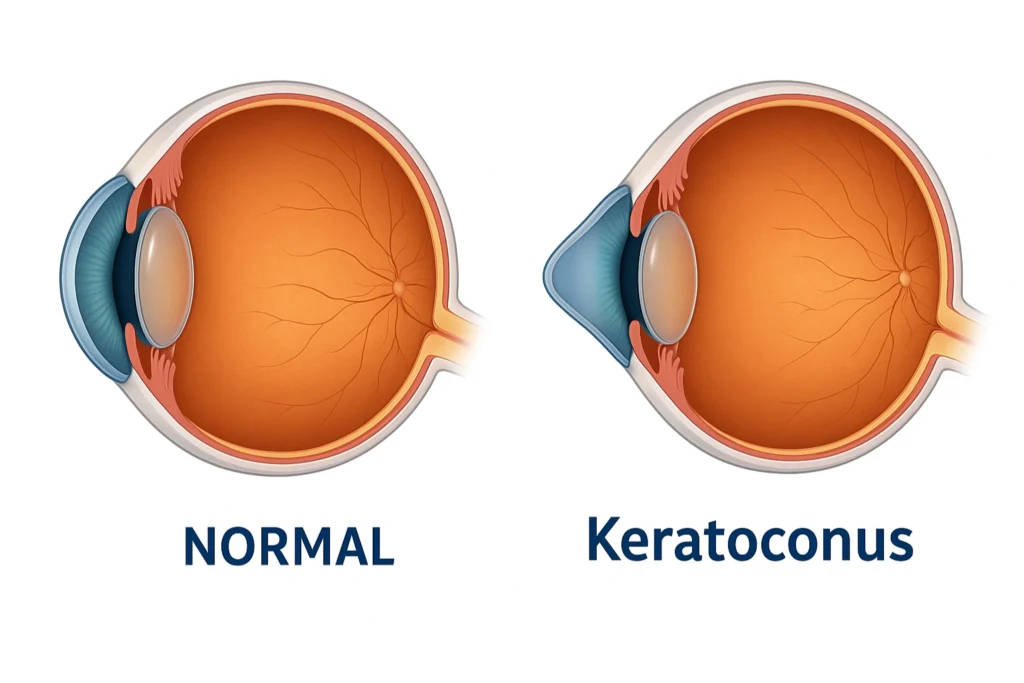
Keratoconus is a progressive thinning and distortion of the cornea, causing it to bulge forward in a cone shape. The result is irregular astigmatism and visual blur that can’t be fully corrected with standard glasses.
The condition often begins in adolescence or early adulthood and can remain mild for years — or progress rapidly. Its course is unpredictable, and that’s why regular monitoring is essential, especially in younger patients.
View VideoContact lenses — from rigid gas permeable to hybrid and scleral designs — can dramatically improve vision by masking corneal irregularities. But even a perfectly fitted lens cannot strengthen the cornea. Behind the clear optics, the disease may still be silently advancing.
View VideoKey Keratoconus Progression Red Flags for Referral
Optometrists and GPs are usually the first line of defence in keratoconus management. The key is not only fitting lenses well, but also spotting the subtle signs that indicate the condition is worsening.
Here are the most important red flags for referral:
1. Rapid Corneal Steepening
An increase in K readings of more than 1 dioptre within 6–12 months is one of the most significant keratoconus progression red flags.
Modern topography and tomography make these changes easy to detect — even before the patient notices symptoms. Comparing scans over time is the most reliable way to catch early deterioration.
2. Younger Age (<25 years old)
Keratoconus tends to behave more aggressively in younger corneas. The collagen is more elastic, and progression can be rapid.
If you see even minor steepening or astigmatic change in a patient under 25, early referral is advised. A short delay can make the difference between being eligible for cross-linking or not.
3. Contact Lens Intolerance or Declining Vision
When patients begin reporting discomfort, shorter wear times, or reduced vision with lenses that previously worked well, the corneal shape has likely changed.
This is a key moment to reassess and consider referral before scarring develops or lens fitting becomes impossible.
4. Corneal Scarring or Hydrops
Visible scarring, stromal haze, or sudden corneal swelling (hydrops) are late-stage signs of biomechanical failure. At this point, only ophthalmic management can prevent further damage or vision loss.

Why Early Detection of Keratoconus Progression Red Flags Matters
Corneal Cross-Linking (CXL) is the only proven treatment to stop keratoconus from progressing. The procedure uses ultraviolet light and riboflavin (vitamin B2) to strengthen the collagen fibers within the cornea, making it more resistant to further distortion.
Clinical studies show CXL can halt progression in around 90% of cases (Wollensak et al., 2003).
However, there’s a catch — it only works while the cornea is still thick and clear enough. Once it thins below about 400 microns or develops scarring, the treatment becomes unsafe or less effective.
That’s why timing is everything. Early referral keeps the window open for cross-linking and gives the patient the best possible chance of long-term stability. Delayed escalation can mean eventual corneal transplantation — an avoidable outcome in many cases.
Shared Care: Working Together for Better Outcomes
Keratoconus management works best when it’s collaborative. Each professional plays an important role:
- Optometrists are ideally positioned to detect early progression through routine imaging and patient feedback.
- General Practitioners can reinforce education about avoiding eye rubbing and managing allergic eye disease.
- Ophthalmologists provide the definitive diagnosis, advanced imaging, and treatments like cross-linking, intracorneal ring segments, or corneal transplantation if needed.
This shared approach ensures that no stage of disease slips through the cracks — from initial detection to long-term stability. Detect keratoconus progression red flags early for the best outcome.
SuppSupporting Patients Along the Way
While clinical management and timely referrals are essential, long-term success in keratoconus often depends on how well patients understand — and participate in — their own care. Education can be the difference between stable vision and avoidable deterioration.
Here are three crucial points every patient should know and every provider should reinforce:
Eye Rubbing Accelerates Progression
Eye rubbing is one of the most powerful and preventable risk factors for keratoconus. The mechanical trauma it causes weakens the already fragile corneal structure, contributing to further thinning and steepening over time.
Patients often rub unconsciously — when their eyes itch from allergies, fatigue, or dryness. It’s important to help them understand that even mild or occasional rubbing can worsen the condition.
Encourage practical alternatives:
- Use prescribed antihistamine or lubricating drops for itch relief.
- Apply a cool compress instead of rubbing.
- Educate family members to gently remind patients (especially children or teens) to avoid rubbing.
Allergy Control Matters
Allergic eye disease is a frequent companion to keratoconus. Chronic inflammation from allergic conjunctivitis or atopic eye conditions leads to itching, which in turn triggers rubbing — creating a destructive cycle.
Proactive allergy management can significantly slow disease progression. Recommend:
- Daily use of antihistamine or mast-cell stabiliser eye drops during allergy seasons.
- Reducing exposure to environmental allergens (dust, pollen, pets).
- Addressing underlying atopy or eczema with the patient’s GP or dermatologist.
When allergies are well-controlled, patients rub less, inflammation subsides, and the cornea remains more stable.
Regular Check-Ups Save Sight
Keratoconus can change subtly over months. Patients may not notice gradual blurring or distortion until the disease has already advanced.
Regular monitoring allows early detection of progression — long before visual function declines.
- Optometrists should schedule corneal topography or tomography at least annually (more frequently for younger or progressing patients).
- Ophthalmologists can compare serial scans to detect even minor changes in corneal curvature or thickness.
Explain to patients that “feeling stable” doesn’t mean the cornea is stable. Even if vision feels stable, since keratoconus progression red flags can develop silently.
Consistent follow-up is what keeps them eligible for sight-saving treatments like cross-linking.
Empowering the Patient to understand keratoconus progression red flags
Empathy and education go hand in hand. Patients with keratoconus often feel frustrated or anxious about fluctuating vision, repeated prescription changes, or the need for specialised lenses.
Take the time to reassure them that:
- Their condition is manageable.
- Early action and discipline can preserve excellent vision for life.
- Support is always available — from their optometrist, GP, and ophthalmologist working as a team.
A few minutes of patient education at each visit can prevent years of visual decline.
The Takeaway
Contact lenses help patients see better — but they don’t stop keratoconus.
If you notice:
- increasing steepness on scans,
- progression in a young patient, or
- growing contact lens intolerance —
it’s time to refer.
Early referral for cross-linking or specialist assessment can preserve vision for life.
Together, optometrists, GPs, and ophthalmologists can make sure keratoconus doesn’t steal sight unnecessarily.


