Managing Glaucoma: Effective Treatments to Protect Your Vision

Discover how to manage glaucoma with treatments such as medications, eye drops, and surgery options. Learn how these treatments can help lower eye pressure and protect your vision from further damage.
Effective Treatments for Diabetic Retinopathy

Diabetic retinopathy can lead to vision loss if untreated. Learn about effective treatments, including anti-VEGF injections and vitrectomy, and how managing blood sugar and blood pressure can help protect your eyesight.
What to Expect During Cataract Surgery Recovery

Cataract surgery recovery is quick, with most patients noticing clearer vision within days. Learn what to expect post-surgery, including tips for healing, managing symptoms, and ensuring a smooth recovery process.
Cataracts Surgery: What to Expect

Cataract surgery is a quick, painless procedure that restores clear vision by replacing the cloudy lens in your eye with an artificial one, ensuring a fast recovery.
Diabetic Retinopathy and Aging: How to Protect Your Eyes as You Get Older

As you age, diabetic retinopathy risks increase. Learn how to protect your vision with early detection, lifestyle changes, and treatment options to preserve eye health.
Glaucoma Progression: Understanding Visual Field Tests
Glaucoma progression is a serious concern when it comes to preserving our precious vision. That’s why visual field tests are crucial in the fight against this silent thief. These tests provide valuable insights into the extent and pattern of vision loss caused by glaucoma.
Visual field tests, also known as perimetry, are diagnostic procedures that assess our entire field of vision, from central to peripheral. By undergoing these tests, we gain a deeper understanding of the impact glaucoma has on our eyesight and can monitor its progression over time.
Keratoconus: Causes, Symptoms, Diagnosis, and Treatment
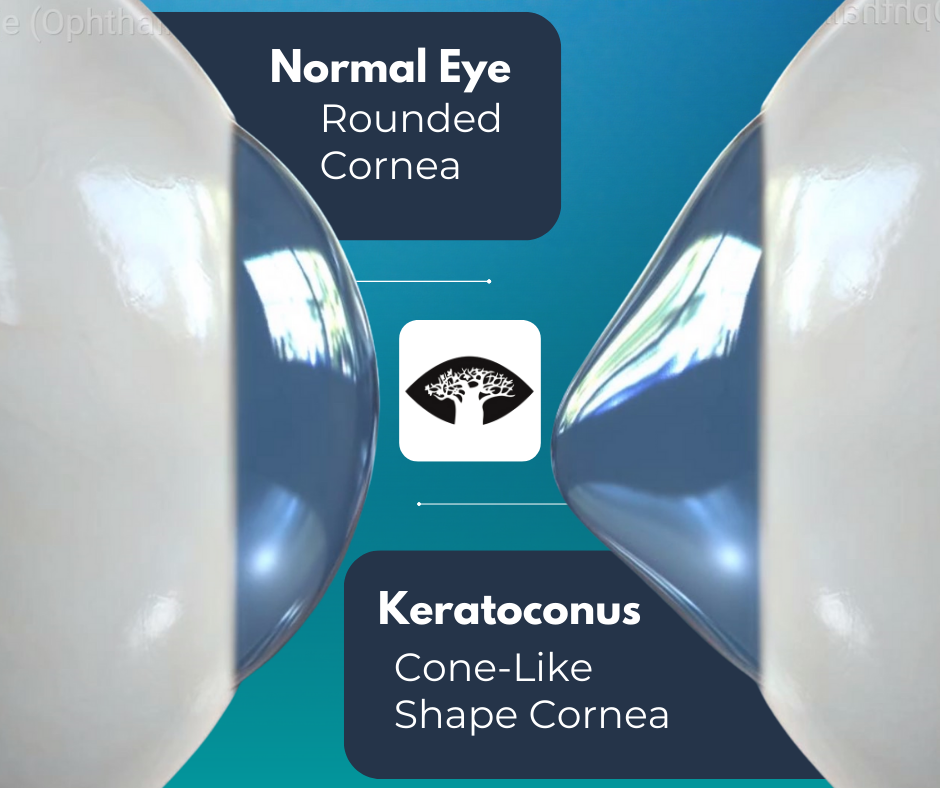
Keratoconus is a progressive eye condition that affects the shape of the cornea, which is the clear outer layer of the eye. In keratoconus, the cornea gradually thins and bulges into a cone-like shape, causing distorted vision, sensitivity to light, and difficulty seeing at night.
Types of Cataracts: Understanding How They Form and Their Symptoms
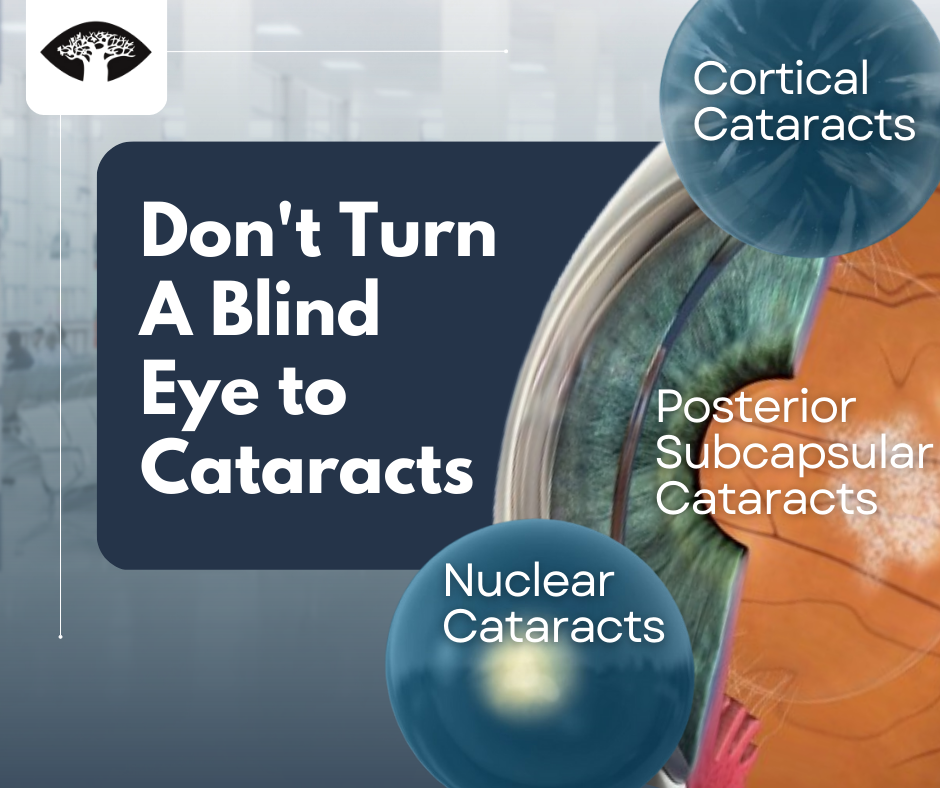
The development of cataracts can be a natural part of aging, but it doesn’t have to mean the end of clear vision. By seeking early diagnosis and treatment from an experienced ophthalmologist, patients can regain their quality of life and continue to enjoy the world around them.
Autoimmune Disorders and Your Eyes: What You Need to Know
As an ophthalmologist, I often see patients who suffer from autoimmune disorders that affect their eyes. These disorders can be complex and debilitating, but with the right knowledge and care, we can help manage them effectively. In this blog post, we will explore the common autoimmune disorders that affect your eyes, how they impact your […]
Navigating Life with Glaucoma: The Importance of Low Vision Rehabilitation
Glaucoma is a progressive eye disease that affects the optic nerve, causing vision loss. It is a leading cause of blindness worldwide, and it is estimated that over 60 million people are affected by glaucoma globally. The disease often goes unnoticed in its early stages, and vision loss can be irreversible if left untreated. Low […]
Restoring Sight and Managing Glaucoma: Glaucoma and Cataract Surgery
Understanding Cataracts and Glaucoma Cataract surgery is a common and highly successful procedure that can help improve vision and quality of life for those suffering from cataracts. However, for those who also have glaucoma, the decision to undergo cataract surgery can be a bit more complicated. In this article, we will explore the potential risks […]
Age Is Not Always A Factor: Discover The Causes Of Early Cataracts
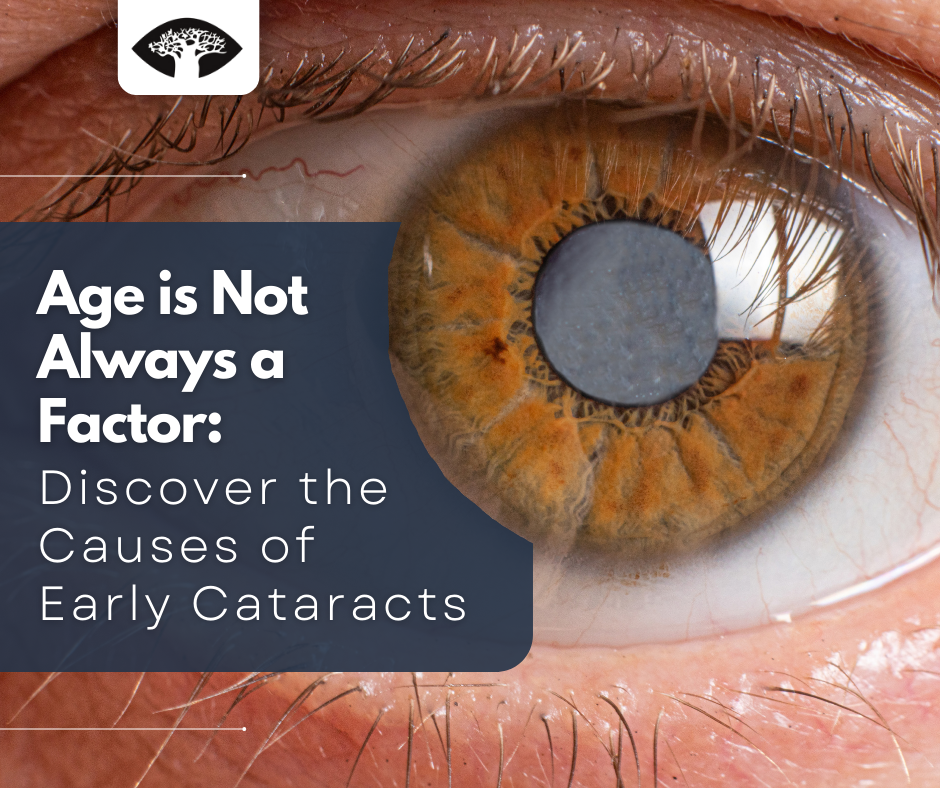
Cataracts are the clouding of the eye’s natural lens, which can lead to vision loss. This clouding can occur gradually over time and is often a normal part of aging. However, cataracts can also develop at an early age due to certain risk factors. It is important to be aware of the causes and symptoms […]
Stress And Your Eyesight

Stress is a normal part of life, but its effects on your mental and physical health can be significant. One of the areas of your body that can be affected by stress is your eyes and vision. While some clinical studies have shown that there can be a link between stress and vision problems. There […]
Don’t Let Dry Eye Put a Damper on Your Day

A Brief Overview Of DED Do you suffer from dry eyes? You’re not alone. Dry eye disease is a common condition that affects millions of people worldwide. It occurs when the eye does not produce enough tears or the tears evaporate to quickly. The tears are important for keeping the eyes lubricated and comfortable, and […]
Everything You Need To Know About Retinal Detachment
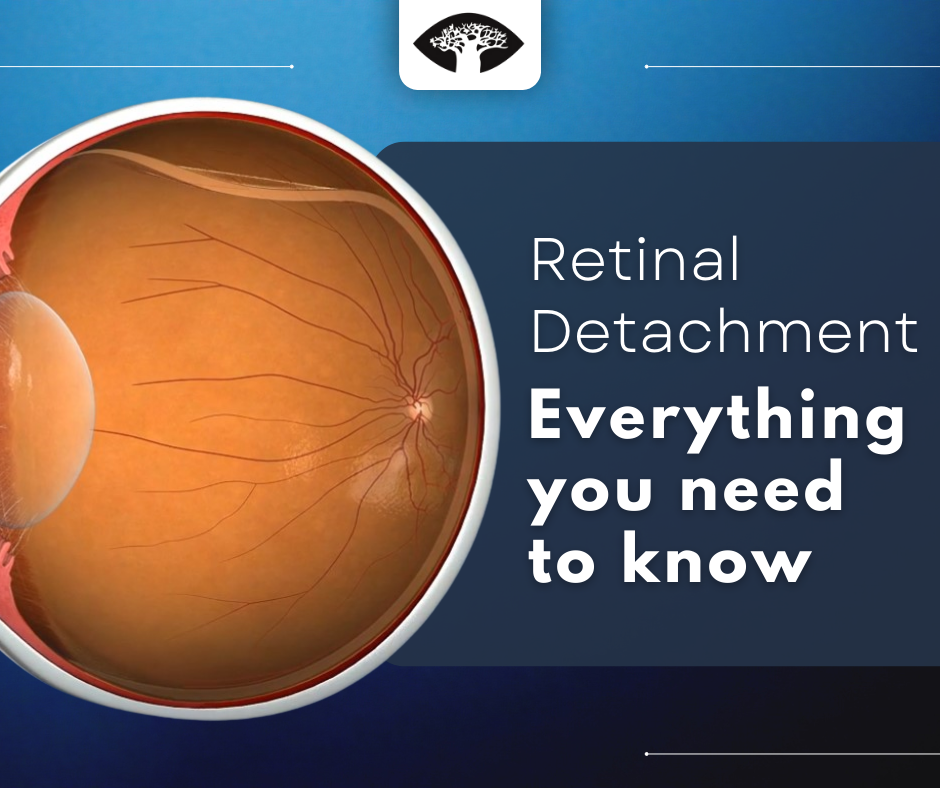
What you need to know Retinal detachment is a medical emergency because if left untreated, it can lead to permanent vision loss. When the retina detaches from the back of the eye, it is no longer able to receive oxygen and nutrients from the blood vessels that surround it. Without these vital nutrients, the retina […]

