Cataracts Surgery Options: Laser vs Traditional
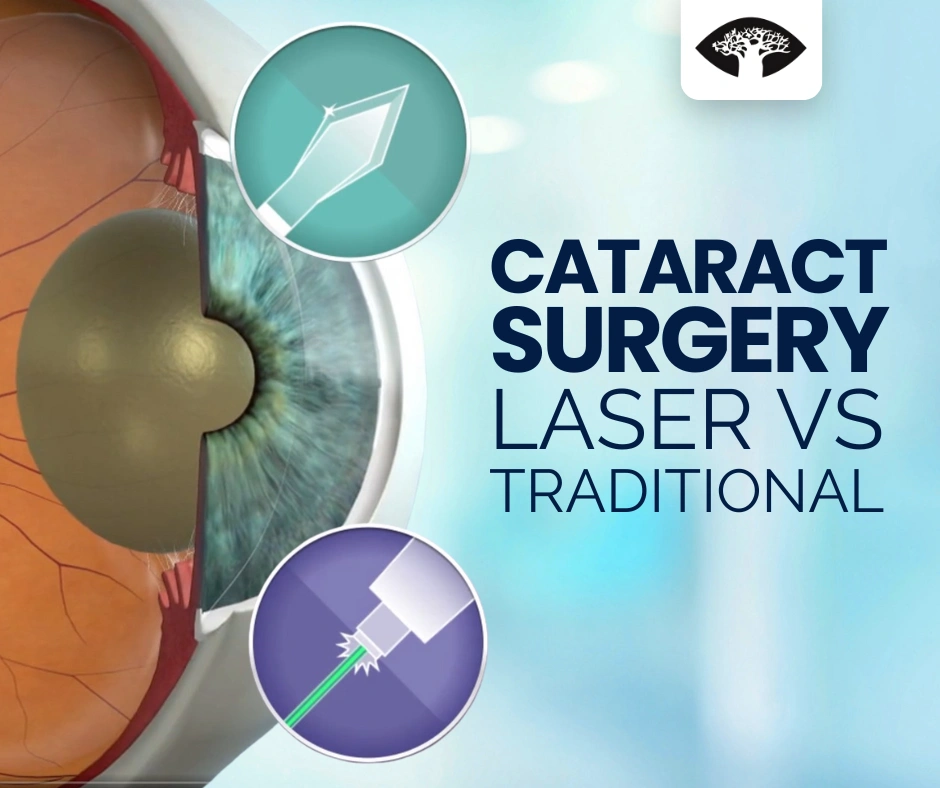
Explore cataracts surgery options, including traditional and laser-assisted techniques, and learn what to expect before, during, and after surgery to restore your vision.
Top 5 Questions to Ask Before Cataract Surgery
Cataract surgery is a safe and effective way to restore vision. Learn the five key questions to ask your ophthalmologist before surgery to ensure the best outcomes for your eye health.
Age-Related Vision Changes: What’s Normal and What’s Not?

As we age, vision naturally changes—but not all changes are harmless. Learn what’s normal, what’s not, and how to protect your eye health well into your golden years.
What is Neuro-Ophthalmology? A Guide to Vision and the Nervous System
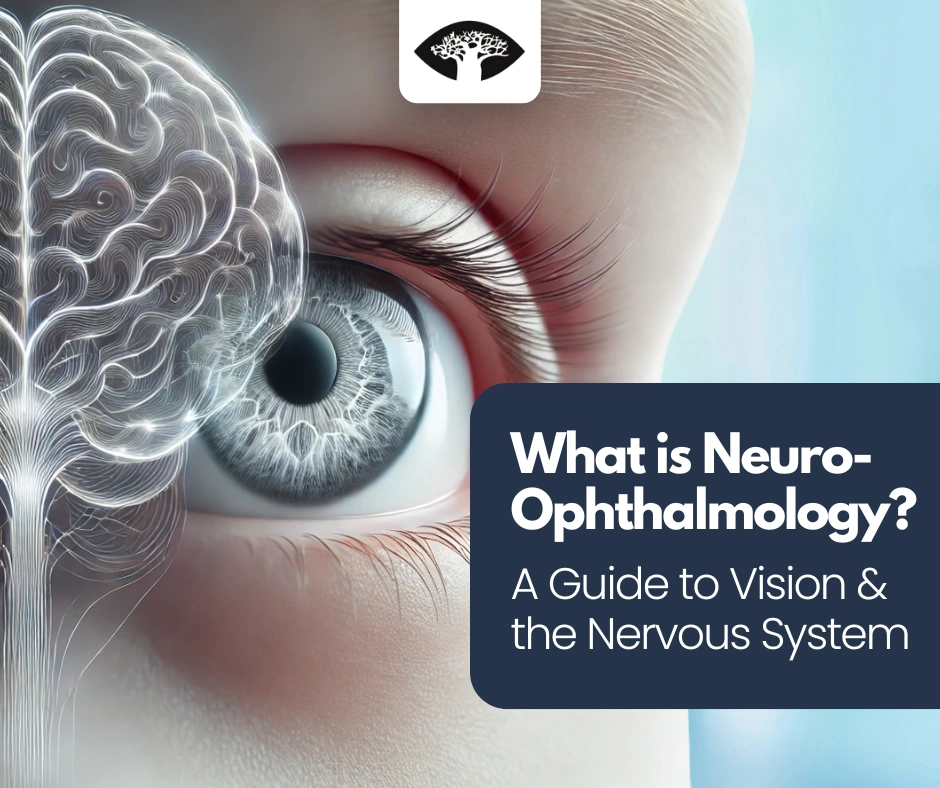
Neuro-ophthalmology focuses on vision problems caused by neurological conditions. It bridges brain and eye health, diagnosing issues like optic neuritis, double vision, and unexplained vision loss for comprehensive patient care.
Optic Neuritis: A Warning Sign for Neurological Conditions?

What is Optic Neuritis? Optic neuritis is a condition that causes inflammation of the optic nerve, which is responsible for transmitting visual signals from the eye to the brain. This inflammation can lead to sudden vision problems, eye pain, and changes in color perception. While optic neuritis can occur on its own, it is often […]
The Importance of Regular Eye Exams for Diabetic Patients
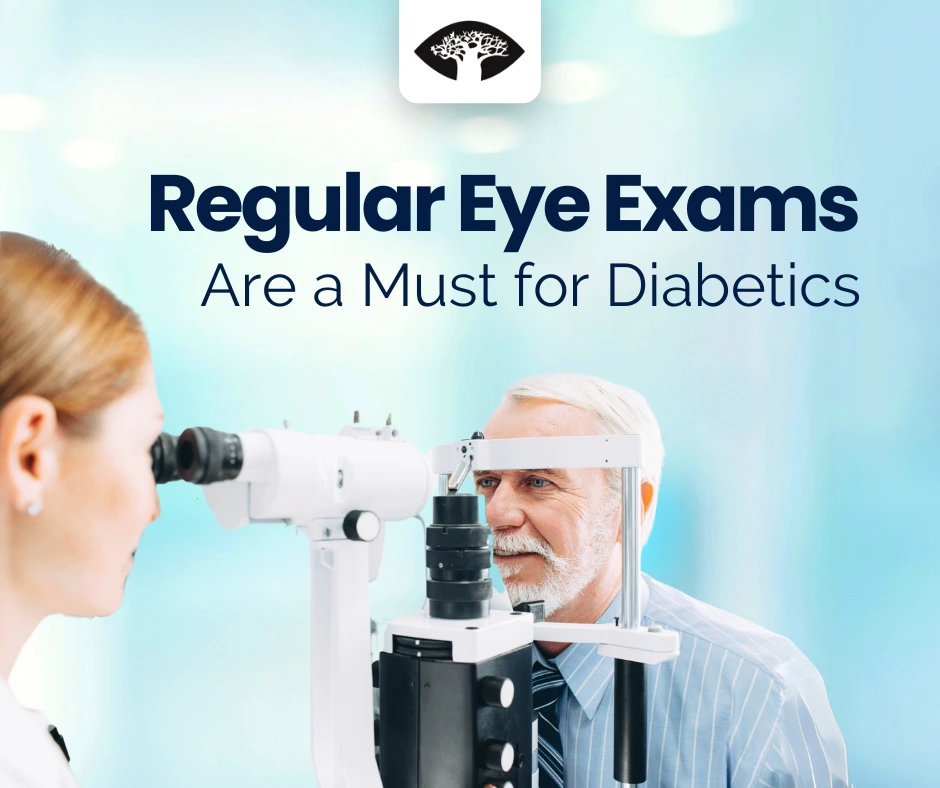
Regular eye exams are essential for diabetic patients, enabling early detection of diabetic retinopathy, monitoring disease progression, and preventing vision loss through timely intervention and personalized treatment plans.
Ocular Infectious Diseases: Prevention, Diagnosis, and Treatment

Ocular infections occur when bacteria, viruses, fungi, or parasites enter the eye, causing redness, pain, or vision problems. Understanding symptoms and seeking early treatment can prevent complications and protect long-term eye health.
The Benefits of Multifocal Intraocular Lenses in Cataract Surgery

Multifocal intraocular lenses improve vision at various distances after cataract surgery, reducing the need for glasses and offering a practical solution for patients seeking clearer, more functional eyesight.
The Role of Genetics in Eye Health: Insights into Family History and Vision Care

Understanding your family’s eye health history is vital. Many eye conditions, like macular degeneration and glaucoma, are hereditary. Early detection, lifestyle changes, and regular check-ups can protect your vision.
Understanding and Managing Age-Related Macular Degeneration (AMD)

Age-Related Macular Degeneration (AMD) is a leading cause of vision loss among individuals over 50, affecting the macula—the central part of the retina responsible for sharp, detailed vision.
How Blue Light Exposure Affects Your Macula

Discover how blue light from screens can strain your eyes and harm your vision over time. Learn simple tips to protect your macula and maintain clear, healthy eyesight.
Floaters and Flashes: When Should You Be Concerned?

Floaters and flashes are often harmless, but sudden changes in vision could signal serious issues like retinal detachment. Learn when to seek help and protect your eyesight effectively.
Cataract Myths and Facts: Separating Truth from Misconceptions

Uncover the facts about cataracts. This article addresses common misconceptions, provides clear insights, and explains how modern treatments effectively restore vision. Understand your options and take control of your eye health.
Understanding the Connection Between Cataracts and Other Health Conditions

Cataracts can be linked to conditions like diabetes, hypertension, and autoimmune diseases. Managing these conditions and regular eye exams are crucial for early detection, preventing progression, and protecting vision health.
Recognizing the Signs of Glaucoma: Early Detection for Lasting Vision

Learn about the early signs of glaucoma, a ‘silent thief of sight.’ Discover symptoms, risk factors, and treatment options to protect your vision with timely, proactive eye care.

