Why Sudden Vision Loss Demands Urgent Action
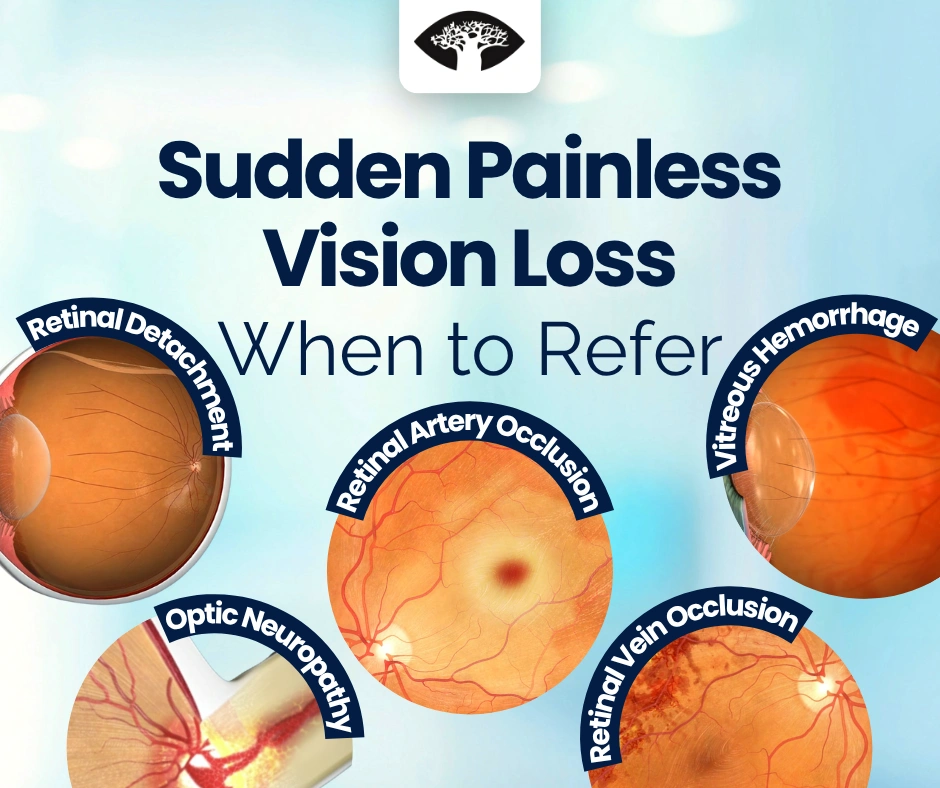
Not every case of visual loss comes with pain — but sudden, painless vision loss is almost always a red flag.
The differential spans retinal vascular occlusions, optic-nerve ischemia, vitreous hemorrhage, and retinal detachment — conditions where minutes or hours can mean the difference between reversible and permanent vision loss.
For front-line clinicians, the message is simple:
Refer immediately. Don’t delay referral for non-urgent tests.
Step-by-Step: First Assessment in Primary or Emergency Care
1️⃣ Measure Visual Acuity and Pupillary Responses
Always document vision in both eyes using best correction.
- Profound monocular loss with a relative afferent pupillary defect (RAPD) suggests optic-nerve or retinal pathology.
- Preserved pupillary reaction with bilateral loss may suggest cortical causes.
2️⃣ Brief Anterior-Segment Check
- Ensure the cornea is clear and there’s no anterior inflammation.
- No pain + clear anterior segment = likely posterior cause.
3️⃣ Basic Systemic Checks
- Record blood pressure and random blood glucose.
- If temporal tenderness, jaw claudication, or scalp pain is reported in older patients → check ESR and CRP immediately (giant-cell arteritis risk).
⚠️ Do not delay ophthalmology contact by ordering CT/MRI or other non-urgent imaging unless advised by the ophthalmologist or stroke team.
Major Causes of Sudden, Painless Vision Loss
1️⃣ Central Retinal Artery Occlusion (CRAO)
Typical features:
- Sudden, profound monocular vision loss (“count-fingers” or worse).
- Pale, opaque retina with a cherry-red spot at the macula.
- May have a small embolus visible at a vessel bifurcation.
Key points:
- Ocular stroke — activate stroke code immediately.
- Coordinate with ophthalmology + neurology.
- Urgent work-up: carotid Doppler, ECG, echocardiogram.
- Manage cardiovascular risk aggressively (BP, lipids, diabetes).
Remember: Retinal ischemia = cerebral ischemia. CRAO patients carry a high risk of concurrent or subsequent brain infarct.
View Video2️⃣ Branch Retinal Vein Occlusion (BRVO)
Typical features:
- Sudden or subacute sectoral vision loss or scotoma.
- Retinal hemorrhages confined to one quadrant (“blood-and-thunder” pattern).
- Risk factors: hypertension, diabetes, hyperlipidemia, glaucoma.
Management:
- Urgent referral for fundus photography and OCT.
- Possible anti-VEGF or laser therapy to prevent macular edema and neovascularization.
- Systemic management of vascular risk factors.
3️⃣ Ischemic Optic Neuropathy (AION)
Typical features:
- Sudden monocular vision loss with pale swollen optic disc.
- Common in patients over 50, often with vascular comorbidities.
- In arteritic AION (GCA) — may have headache, scalp tenderness, jaw claudication, or polymyalgia.
Immediate steps:
- If GCA suspected: start systemic corticosteroids immediately, even before lab confirmation.
- Order ESR, CRP, and platelet count.
- Coordinate with ophthalmology for urgent temporal artery biopsy and visual-field testing.
Non-arteritic AION: related to nocturnal hypotension, diabetes, or small crowded discs — requires systemic evaluation and risk modification.
4️⃣ Vitreous Hemorrhage
Typical features:
- Sudden visual obscuration or “dark red haze.”
- May see moving shadows or cobwebs.
- Fundus view may be obscured on ophthalmoscopy.
Likely causes:
- Proliferative diabetic retinopathy, retinal tear, trauma, or posterior vitreous detachment.
Next steps:
- Avoid dilating delay — refer for urgent B-scan ultrasound to exclude retinal detachment.
- Treat the underlying cause (laser, vitrectomy if non-clearing).
5️⃣ Retinal Detachment
Typical features:
- Flashes, floaters, or a “curtain” descending over vision.
- Usually unilateral and painless.
- Visual acuity depends on macular involvement.
Management:
- Surgical emergency. Early repair (within hours to days) offers the best prognosis.
- Instruct patient to keep head still and avoid eye pressure until seen by ophthalmologist.
Other, Less Common Causes
- Occipital stroke: Bilateral or homonymous loss with normal ocular exam.
- Optic neuritis: Pain on movement + young age — usually not painless, but occasionally subtle.
- Posterior uveitis / macular hemorrhage: May mimic painless loss; needs specialist imaging.
When to Call Immediately — Practical Algorithm
1️⃣ Check visual acuity and RAPD.
2️⃣ Assess retina and optic disc if visible.
3️⃣ Measure BP and glucose (ESR/CRP if GCA suspected).
4️⃣ If CRAO or AION suspected → treat as stroke / arteritis emergency.
5️⃣ Call ophthalmologist immediately for any posterior cause — do not delay with non-urgent imaging.
6️⃣ Document onset time, associated symptoms, systemic risks, and vision level.
⏱️ Time = Retina.
Early recognition and referral are the only modifiable factors in most causes of painless visual loss.
Systemic and Neurological Coordination
- CRAO patients should enter stroke pathways for urgent carotid and cardiac evaluation.
- AION (arteritic) requires coordination with rheumatology or internal medicine for systemic steroid therapy.
- BRVO and vitreous hemorrhage often uncover poorly controlled diabetes or hypertension, warranting ongoing medical follow-up.
Key Takeaway
Sudden, painless loss of vision is an ophthalmic emergency, not a routine referral.
Your role as a primary or emergency clinician is rapid triage and direct referral, not delayed work-up.
Retinal artery occlusion, ischemic optic neuropathy, retinal detachment, and vitreous hemorrhage each demand urgent ophthalmic assessment — and in the case of CRAO, activation of a stroke protocol.
When in doubt, refer first and investigate later.
Timely communication can mean the difference between vision preserved and vision lost.